Randevu +90 324 238 83 83
Home »
Last updated on August 27th, 2024 at 12:31 am
Home »
In the early stages of diabetic retinopathy, you may not have symptoms. As the condition progresses, you may develop:
Careful management of your diabetes is the best way to prevent vision loss. Especially, if you have diabetes, see your eye doctor for an annual eye exam, even if your vision looks good.
Particularly, developing diabetes while pregnant (gestational diabetes) or having diabetes before becoming pregnant can increase your risk of diabetic retinopathy. If you are pregnant, your eye doctor may recommend additional eye exams throughout your pregnancy.
Also, contact your eye doctor right away if your vision suddenly changes or becomes blurry, spotty or hazy.
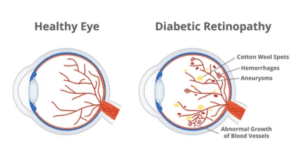
Over time, having too much sugar in your blood can cause the tiny blood vessels that feed the retina to become clogged and cut off blood flow. As a result, the eye tries to form new blood vessels. But these new blood vessels do not develop properly and can leak easily.
In this more common form, call non-proliferative diabetic retinopathy (NPDR), new blood vessels do not grow (proliferate).
Especially, when you have NPDR, the walls of the blood vessels in your retina weaken. Small projections protruding from the walls of small vessels, sometimes leaking fluid and blood into the retina. Larger retinal vessels may also begin to dilate and become irregular in diameter. NPDR can progress from mild to severe as more blood vessels become blocked.
Sometimes retinal blood vessel damage leads to fluid buildup (edema) in the central part of the retina (macula). If macular edema reduces vision, treatment is require to prevent permanent vision loss.
Especially, diabetic retinopathy can progress to this more severe type known as proliferative diabetic retinopathy. In this type, damaged blood vessels close, causing new, abnormal blood vessels to grow in the retina. These new blood vessels are fragile and can leak into the clear, jelly-like substance that fills the center of your eye (the vitreous).
Eventually, scar tissue from the growth of new blood vessels can cause the retina to detach from the back of the eye. Also, pressure can build up in the eyeball if new blood vessels interfere with the normal flow of fluid in the eye. Therefore, this buildup can cause glaucoma by damaging the nerve (optic nerve) that carries images from your eye to the brain.
Anyone with diabetes can develop diabetic retinopathy. The risk of developing an eye condition may be increased as a result of:
Diabetic retinopathy involves the growth of abnormal blood vessels in the retina. Complications can lead to serious vision problems:
Particularly, new blood vessels can bleed into the clear, jelly-like substance that fills the center of your eye. If the amount of bleeding is small, you may only see a few dark spots (flying objects). In more severe cases, blood can fill the vitreous cavity and completely block your vision.
Vitreous hemorrhage alone does not usually cause permanent vision loss. The blood usually clears from the eye within a few weeks or months. Unless your retina is damaged, your vision will likely return to its former clarity.
The abnormal blood vessels associated with diabetic retinopathy stimulate the growth of scar tissue, which can pull the retina away from the back of the eye. Also, this can cause floating spots in your vision, flashes of light, or severe vision loss.
New blood vessels can grow in the front of your eye (iris) and block the normal flow of fluid in the eye. Therefore this is causing pressure in the eye. Also, this pressure can damage the nerve (optic nerve) that carries images from your eye to the brain.
Particularly, diabetic retinopathy, macular edema, glaucoma, or a combination of these conditions can cause complete vision loss. Especially if the conditions are poorly manage.
Generally, you can’t always prevent diabetic retinopathy. However, regular eye exams, good control of your blood sugar and blood pressure, and early intervention for vision problems can help prevent serious vision loss.
If you have diabetes, reduce your risk of developing diabetic retinopathy by doing the following:
Manage your diabetes. Make healthy eating and physical activity part of your daily routine. Try to do at least 150 minutes of moderate aerobic activity, such as walking, each week. Take diabetes medications or insulin as directed.
Monitor your blood sugar level. Also, you may need to check and record your blood sugar levels several times a day or more often if you are sick or under stress. Ask your doctor how often you should test your blood sugar.
Also, ask your doctor about the glycosylated hemoglobin test. Specifically, the glycosylated hemoglobin test, or hemoglobin A1C test, reflects your average blood sugar level for the two to three months before the test. For most people with diabetes, the A1C goal is to be below 7%.
Especially, keep your blood pressure and cholesterol under control. Eating healthy foods, exercising regularly, and shedding extra pounds can help. Sometimes medication is also needed.
Moreover, if you smoke or use other forms of tobacco, seek help from your doctor to quit. Especially, smoking increases your risk of various diabetes complications, including diabetic retinopathy.
Pay attention to vision changes. Particularly, if your vision suddenly changes or becomes blurry, mottled or hazy, contact your eye doctor right away.
Remember, diabetes does not necessarily lead to vision loss. Therefore, taking an active role in diabetes management can go a long way in preventing complications.
Diabetic retinopathy can be diagnose with a comprehensive eye exam. The drops place in your eyes for this examination will enlarge (dilate) your pupils and allow your doctor to see inside your eyes better.
During the exam, your eye doctor will look for abnormalities in the inner and outer parts of your eyes.
After your eyes are open, dye is injected into a vein in your arm. Pictures are then taken as the dye travels through the blood vessels of your eyes. Images can pinpoint closed, broken, or leaky blood vessels.
With this test, pictures provide cross-sectional images that show the thickness of the retina. This will help determine how much fluid, if any, is leaking into the retinal tissue. It will then be follow up with OCT tests to monitor how the treatment is progressing.
Treatment, which depends largely on the type of diabetic retinopathy you have and how severe it is, is aimed at slowing or stopping the progression.
If you have mild or moderate non-proliferative diabetic retinopathy, you may not need treatment right away. However, your eye doctor will watch your eyes closely to determine when you may need treatment.
Work with your diabetes doctor (endocrinologist) to determine if there are ways to improve your diabetes management. When diabetic retinopathy is mild or moderate, good blood sugar control can often slow progression.
If you have proliferative diabetic retinopathy or macular edema, you will need emergency treatment. Depending on specific problems with your retina, options may include:
Injecting medication into the eye. These drugs, call vascular endothelial growth factor inhibitors, are inject into the vitreous of the eye. They help stop the growth of new blood vessels and reduce fluid buildup.
These drugs are injecting with topical anesthetic. Injections may cause mild discomfort such as burning, tearing or pain 24 hours after injection.
These injections will need to be repeatedly. In some cases, the drug is use in combination with photocoagulation.
Also known as focal laser therapy, this laser therapy can stop or slow the leakage of blood and fluid in the eye. Leakages from abnormal blood vessels during the procedure are treat with laser burns.
It’s usually apply in a single session at your doctor’s office or eye clinic. If you had blurred vision from macular edema prior to surgery, treatment may not return your vision to normal, but it will likely reduce the chance of your macular edema worsening.
Also known as scatter laser therapy, this laser treatment can shrink abnormal blood vessels. During the procedure, areas of the retina distal to the macula are treat with scattered laser burns. Burns cause abnormal new blood vessels to shrink and scar.
Particularly, these procedures are done in two or more sessions at the Eye Clinic in a hospital. Also, your vision will be blurry about a day after the procedure. Although, some loss of peripheral vision or night vision is possible after the procedure.
This procedure uses a small incision in your eye to remove blood from the middle of the eye (vitreus) and scar tissue that draws the retina. Also, it is perform in a surgery center or hospital using local or general anesthesia.
Especially, treatment can slow or stop the progression of diabetic retinopathy, but it is not a cure. Because diabetes is a lifelong condition, retinal damage and vision loss are still possible in the future.
More importantly, you will still need regular eye exams even after diabetic retinopathy treatment. Also, at some point, you may need additional treatment.
Vitrectomy Retina Surgeries, Strabismus Crossed Eye Squint Treatments, Macular Degeneration Treatments. Glaucoma Disease and Treatments. Retinitis Pigmentosa Disease and Treatments. Dry Eye Syndrome Treatments. Periodic Eye Examinations.
Randevu +90 324 238 83 83
